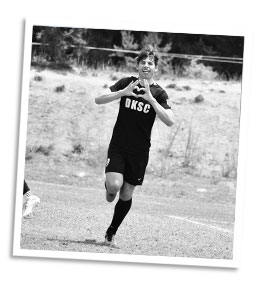
Luke Myers
Luke is a student at John Paul II High School in Plano, TX and competitive soccer player with his DKSC U17ECNL team. He has always been a very athletic kid and also played flag football, basketball, track and field, futsal, tennis and golf, but soccer has remained his #1 passion through the years and he wants to play collegiately. In June of 2021, Luke had his yearly physical and was offered an EKG by his PA, who mentioned the story of another soccer player collapsing on the field. After the EKG was performed, Luke’s PA returned to let his family know the results were abnormal, and recommended either a Living for Zachary Heart Screening or that his family see a pediatric cardiologist. Right after they left the office, Luke’s mother scheduled an appointment for a Living for Zachary Heart Screening in Denton and took him in for the screening the next day.
While away on a family trip, Luke’s family received the results of his screening: he had been diagnosed with Wolff-Parkinson-White Syndrome. “We didn’t know much about it and Googling didn’t help – we were scared and concerned,” said Luke’s mother, Mary Claire.
An appointment was immediately scheduled with Dr. Alan Chin-Pao Sing at Children’s Hospital Plano in July 2021, who did another EKG and discussed the findings with Luke’s family. They were referred to electrophysiologist Dr. William Scott, who helped them decide to move forward with an electrophysiology study on Luke’s heart. The electrophysiology study/catheter ablation supra-ventricular procedure was scheduled and performed in November 2021. Dr. Scott found the culprit, ablated it, and Luke was home by 4:00pm that day. Three days later, he was back on the soccer field. He will continue to undergo yearly heart checks for the next several years.
“I am a huge proponent for all kids to get these screenings…even when there is no history in the family or reason to believe that there is anything wrong. We had no clue about this abnormality existing within Luke, but once we did we were so grateful to have prevented something tragic and or life changing for all of us. We thank God daily for the Living for Zachary Screening.” -Mary Claire Myers

Camden Thrailkill
Camden Thrailkill is a young man from Denton Guyer High School who is extremely passionate about playing football and baseball. Camden has played sports competitively since he was in middle school and has broken many records. His love and dedication to these sports has allowed him to focus on the ultimate goal of playing at the collegiate level!
Growing up, Camden has always been a very healthy kid. He received his yearly physical and attended his annual doctor visit in order to participate in school sports. He was like any other normal, healthy kid and never showed any signs of health issues. In August 2016, Living for Zachary partnered with The Heart Hospital Baylor Denton to offer free heart screenings to the Denton Guyer football team. A few days later Camden and his family found out that he had an isolated cleft of the mitral valve. None of the yearly physical exams had ever or would have ever caught this rare heart condition. “Not only was he symptom-free and always healthy, but he was born with this heart defect and it went undetected his entire life,” said his mother, Liz.
Camden received robotic arm surgery in October 2016 at The Heart Hospital Baylor Plano and was back in school three weeks later. He tried out for the high school’s baseball team in January 2017 and made the team! “My heart is never going to hold me back,” said Camden.
Today, Camden is back to being a completely healthy young man and has gone on to play baseball at the next level at Navarro College.
“I promise to make my second chance count. Count in my relationship with God. Count in my relationship with my family! Count in my academics and my athletics and I will always honor the ones who sacrificed to give me this opportunity.” -Camden

Makenzie Wise
Makenzie Wise complained of rapid heartbeat, chest pain, and shortness of breath and her parents took her to the pediatrician for an exam. The pediatrician felt her symptoms were most likely due to high school stress, but encouraged Makenzie to be screened to rule out any heart issues. On December 29, 2014 Makenzie’s parents made an appointment for the 15-year-old to have a Living for Zachary Heart Screening at The Heart Hospital Baylor Plano (THHBP) over Christmas break. A few weeks earlier, their friend posted a photo of her son getting his heart screened, which prompted the Wise family to take Makenzie to do the same.
On Saturday, January 3, 2015 (three days later), Dr. David Rawitscher at THHBP phoned Makenzie’s mom Lari, and said that Makenzie has WPW (Wolff-Parkinson-White syndrome). He told her that Makenzie needed to stop all physical activity and seek medical attention immediately for impending surgery. Lari began to feel anxious. She and her husband prayed for guidance, wisdom, and peace prior to sharing the information with Makenzie.
As expected, Makenzie’s initial reaction was fear, primarily due to her inability to dance on the drill team, Clark High School Cougarettes, as they were preparing for competition season. She also recalled knowing about heart procedures from watching many episodes of Grey’s Anatomy which caused her to feel overwhelmed by the idea of open heart surgery. She was relieved to know she would most likely be having an arterial ablation, which was not open heart surgery.
The family met with Dr. Zeltser at Children’s Hospital within two days of Makenzie’s diagnosis. She explained the significance of Makenzie’s condition and the urgency to get her into surgery. The family shared Makenzie’s desire to try out for the Planoette High School drill team in less than three weeks, so Dr. Zeltser expedited the surgery for the following morning. Makenzie and her parents had little time to even think about what was about to occur, let alone be fearful.
After Makenzie’s surgery, Dr. Zeltser said Makenzie’s case was challenging, but she felt she had solved the problem. The family later learned from testing the electricity in Makenzie’s heart that her condition was severe and more than likely would have caused Sudden Cardiac Arrest (SCA).
Within four days Makenzie was back at school and tried out for the Planoettes. She successfully made the team!
Mackenzie and her family were so thankful and relieved that she had her heart screened. Her mom couldn’t wait to share their appreciation with Karen Schrah (Zac’s mom) for starting the Living for Zachary organization and promoting heart screenings. To this day, the family constantly shares their story with others and encourages other parents to have their children’s heart screened.
“We thank God for Zachary and his mom Karen every day.” –Lari Wise

Jackson Dakuginow
Jackson Dakuginow of Plano first heard about the Living for Zachary heart screening from a friend on his baseball team. In August of 2014, his mother Cathy Jo took the 12-year-old and his 14-year-old sister Annabelle to Walgreens to have a Living for Zachary heart screening. A phone call confirmed that Annabelle’s test results were normal, but Jackson’s echocardiogram showed an abnormality in his aortic valve.
Cathy Jo took Jackson to the pediatrician who confirmed that he has a bi-cuspid aortic valve. That is when the aortic valve, which is supposed to have three sections (tri-valve), only has two. It does not typically adversely affect a young person, but it later can lead to a leaky valve and cause an enlarged heart. Cathy Jo recalled that her maternal grandfather died at age 57 from an enlarged heart and also had a bi-cuspid aortic valve. Now that she is aware that this is a hereditary condition and more prevalent in males, she will also have her younger son screened when he is older.
Thanks to the Living for Zachary Heart Screening, Jackson and his family now know that he needs to have his heart checked every year. Being aware of his condition and monitoring it can help prevent further issues. Jackson’s physical activity is not limited, but he needs to remember to get medical attention if experiencing any symptoms such as fatigue or shortness of breath.
Cathy Jo is grateful for having had her children screened.
“I’m a big proponent of what Living for Zachary does.” –Cathy Jo

Mike Reisinger
In 2011, Mike was sitting in service at St. Mark’s Catholic Church when he collapsed with little warning. Thankfully, that wasn’t the end of Mike’s story.
Just one year prior, Living for Zachary had made its first-ever AED donation to St. Mark’s – and that AED was quickly retrieved as a bystander performed CPR on Mike. The AED was used to shock Mike’s heart back into rhythm, saving his life. Since that day, Mike has dedicated himself to making sure each and every citizen is prepared to help in the case of an emergency just like his. He serves as a CPR/AED instructor and is a champion of Living for Zachary’s mission.
Our first-ever AED donation quickly became so much more than that: it gave the gift of a second chance to Mike and his family.

Coach Tom Rapp
Just over ten years after the loss of Zac Schrah at a Plano East Panthers football practice, his impact became tangible in a whole new way as a life was saved in that same spot with the team he loved.
In August of 2019, Coach Rapp was heading back to the indoor facility at Plano East Senior High School after an outdoor practice when he suddenly collapsed behind the baseball field fence. Upon recognizing Coach Rapp was in need of immediate help, coaches and trainers sprang into action, determined to use their knowledge and tools to not let history repeat itself. While one coach called 911, a trainer performed CPR and an AED was retrieved and used on Coach Rapp within minutes. An ambulance arrived and transported Coach Rapp to the hospital where he received an implantable cardioverter defibrillator. Within the span of a few weeks, Coach Rapp was back to coaching with a new perspective on how the life and legacy of one young man could make such a difference.
Coach Nate Collins, who called 911 after Coach Rapp’s collapse: “The first thing I thought about was, ‘Wow, is this not full circle?’ Because after Zac, after Coach Rapp, that work is directly saving lives.”

Joshua Rester
Since Joshua Rester was a little boy, he has loved soccer, math, science and physics. He was excited when he was accepted into the engineering program at the University of Texas at Austin and decided to pursue a dual major in Mechanical Engineering and Radiation Physics.
The summer before Joshua started college he got a job at Schlitterbahn in New Braunfels, Texas as a lifeguard. He loved it! Every summer he couldn’t wait until he could get back to Schlitterbahn. Like his studies, Joshua took his job very seriously and soon moved up in the ranks, becoming a Lifeguard Instructor and Supervisor. This past May he was back at Schlitterbahn making sure his new lifeguards were properly trained in life saving techniques by teaching them First Aid and CPR.
On July 1, 2013, Joshua started his day, like any other day, up at 6:00 a.m. and off to Schlitterbahn! He started that day performing an audit on his team to ensure they were safety ready. Shortly after, Joshua started to feel funny. As he started to walk over to the Lifeguard Rest Area, he called First Aid over the walkie-talkie and asked them to come examine him. When Joshua got to the rest area, he started talking to one of his lead lifeguards about the plan for the day, and in mid-sentence he dropped to the ground. The lead lifeguard thought it was another audit and blew his whistle as though it was a real emergency. Two lifeguards immediately responded and along with the lead lifeguard started performing the audit. Almost immediately, they realized this was for real – Joshua was not breathing and did not have a pulse. One of the lifeguards immediately called a “code 604U” (which is equivalent to a code blue) and began CPR. Within seconds, several other lifeguards and supervisors arrived and began the rotations of compressions and artificial respiration. First Aid arrived about the same time as the “604U” was called and started attaching the Automated External Defibrillator (AED) to Joshua. Within 90 seconds from when Joshua’s heart stopped, the first shock was delivered. Though he still wasn’t breathing, they were able to detect a faint pulse. When the ambulance arrived, the EMTs immediately took over performing CPR and called for Air Life to meet them at the local hospital a mile away.
On the second day in the local hospital’s ICU, Joshua’s family was told that he went into ventricular fibrillation, a form of Sudden Cardiac Arrest (SCA). His doctors said that less than 8% of people that experience this survive and even fewer survive without permanent damage. Joshua has had many physicals throughout his life and never exhibited any signs of having a heart condition, nor has there been any history of heart problems in his family. Joshua’s doctors have installed an implantable cardioverter-defibrillator (ICD) into his heart to protect him if this occurs again. Joshua was diagnosed with Long QT Syndrome (LQTS).
Joshua is alive today because of the quick response and use of an AED by his colleagues. The best part of the story: several of the lifeguards that saved Joshua were also trained by him. Kristen Boggess and Wilson McDonald played a key part in saving Joshua’s life. They were awarded the Hero at Heart award at the 2015 Living for Zachary HeartBeats Gala.
Joshua recently graduated from the University of Texas Austin and now works as a Nuclear Project Engineer in Atlanta, GA.

Dylan Cheatham
Dylan Cheatham was a healthy kid who played soccer since the age of four. Like most kids, he had his yearly physical at the pediatrician’s office and never encountered any health problems.
On April 15, 2009, his mother Malissa was at home in Melissa, TX as the 13-year-old was outside throwing a football with neighborhood friends in the yard. Suddenly one of the boys ran in and said something was wrong with Dylan. Malissa went outside to find Dylan sitting on the ground with his back propped up against another friend’s legs. “I took one look at him and just knew something was wrong,” says Malissa. She called 911 and was told the ambulance would take 10 minutes to arrive. Fortunately, a police officer who happened to be in the area responded. He told Dylan to lay back and Dylan turned as pale as a ghost. The officer did CPR until the ambulance arrived. They shocked him with a defibrillator but could not stabilize him, so they took him to the hospital in McKinney where they were met by a Care Flight helicopter that transported him to Children’s Hospital.
In the Cardiac Intensive Care Unit at Children’s the doctor told his family that Dylan might not survive through the night. He was put on life support, made it through the night and was kept on the life support machine for the next few days. Meanwhile, his parents prepared for the worst.
Five days later, Dylan was weaned off of life support and his medicines were decreased to bring him out of an induced coma. Dylan was fitted with an Implantable Cardioverter-Defibrillator (ICD) to control his heart beats. He spent a total of 38 days in the hospital.
In 2013, Dylan’s ICD activated three times in three weeks and shocked him. He was referred to the Oklahoma University Medical Center in Norman where, during an 8-hour surgery, a doctor burned out over 30 areas within Dylan’s heart that were causing his arrhythmias.
While on life support, the machine limited oxygen to the muscles in Dylan’s right leg. He had surgery to ease the pain, but at the end of 2014, Dylan made the decision to amputate his leg six inches below the knee to alleviate the severe pain. Though SCA changed his life, Dylan is one of the fortunate few who has been able to go on to share his story and life-saving message with others.

Callie Banks
Callie was an avid volleyball player playing both at the Club Level as well as on the Allen High School Volleyball team. On September 21, 2010 while playing in a high school volleyball game Callie collapsed on the court and had no pulse. Angels were watching over her that night as a physician, two trauma nurses and an off duty EMT/fire fighter happened to be in the audience. CPR was started within seconds, and an AED was applied twice by the physician in attendance, then again by the paramedics when they arrived. Callie was care-flighted to Children’s Hospital and spent 10 days in the hospital. Before leaving the hospital she was implanted with a dual defibrillator/pacemaker to control the arrhythmias. While in the hospital many cardiac tests were performed, but doctors did not have a diagnosis. In December, 2010 through genetic testing Callie was diagnosed with Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy (ARVD/C). This is a degenerative, incurable form of heart disease. In this disease, the right ventricle is affected as the heart muscle is replaced with fibrous tissue, which triggers the arrhythmia.
In 2014, Callie was awarded the Living for Zachary Academic Scholarship as she pursued a degree in healthcare at Auburn University to make a difference in the lives of others.
Brock Cullers
In the fall of 8th grade when Brock was 13, he played on his school’s football team. After a hard-hitting tackle, his heart began to race; this happened on two different occasions on the practice field. He mentioned the first incident to his coach and his father, but because he appeared to be in perfect health, had annual physicals with no known familial heart issues, the event was dismissed. The second time his heart raced, Brock kept it to himself.
Yet on February 4, 2008, at the age of 14, Brock experienced these symptoms again. Not only were his symptoms the strongest and most difficult to endure up to that point, they also lasted over 20 minutes. Gratefully his dad was there to witness it, alarmed at Brock’s pulse racing 200-300 beats per minute as he sat still. He was taken to the emergency room and an EKG identified the cause. The diagnosis was Wolff-Parkinson-White syndrome, which has a side effect of sudden cardiac arrest. All physical activity was stopped, and teachers were notified of his condition in case an incident occurred during class. A few weeks later, he had heart surgery at Children’s Hospital where an ablation was successfully performed. To date, he continues to be symptom-free.

Kylee Shea
Kylee Shea was a seemingly healthy 12-year-old in 7th grade attending Mause Middle School in Frisco, TX. On September 26, 2011, Kylee was running late for gym class. While hurriedly trying to get there, she suddenly noticed she was feeling light headed and just not right. She stopped to take a seat and that’s the last she remembers. Surveillance cameras located in her school hallway later revealed the entire story. Upon sitting down, Kylee collapsed. Two coaches came rushing to her aid after being alerted by startled students. Coach Brent Reese immediately began CPR as Coach Kristen Goodgion grabbed the school’s Automated External Defibrillator (AED). Fortunately, the coaches were trained in using the AED and administered two shocks. Emergency personnel arrived, and Kylee was airlifted to a local hospital for further treatment. Doctors determined that Kylee had an undetected heart condition, and she was implanted with an Implantable Cardioverter-Defibrillator (ICD). Doctors estimate that without the rapid response of Goodgion and Reese and the use of the AED, Kylee would have had just a 3% chance of surviving her episode of heart arrhythmia, and only a 1% chance of surviving without brain damage. Kylee is now a thriving teenager that enjoys theater classes and plans to pursue this in her bright future. Most of all, she lives life as a teenager who greatly appreciates being able to spread this vital message: Being aware and prepared save lives!
